Welcome to Helping Mothers Have Healthy Babies
Sarah Wells, University of Delaware
Background
Infant mortality is described as the death of a child before the age of one year. Understanding the infant mortality rate (IMR) is key to comprehending the overall health of a society and looking into infant mortality can give a window into the quality of healthcare provided in a given population. It can be seen as an indicator of community health status, poverty, and socioeconomic status levels in the community, and of the healthcare and medical services provided within the community.
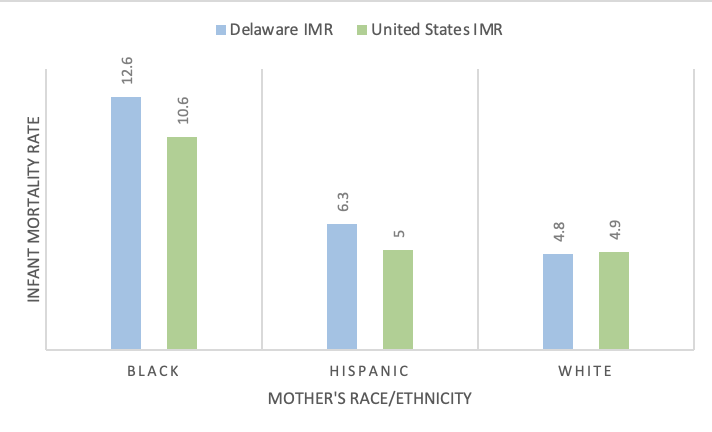
Delaware has an IMR of 7.0 deaths per 1,000 live births. This is significantly higher than the US national average of 5.7. Along with the rest of the country, Women of Color in the State of Delaware face higher rates of infant mortality as opposed to their White counterparts. The rate for non-Hispanic Black women in Delaware is 12.6 deaths per 1,000 live births, which is higher than the national average, as opposed to White women, whose rate is only 4.8 deaths per 1,000 live births.
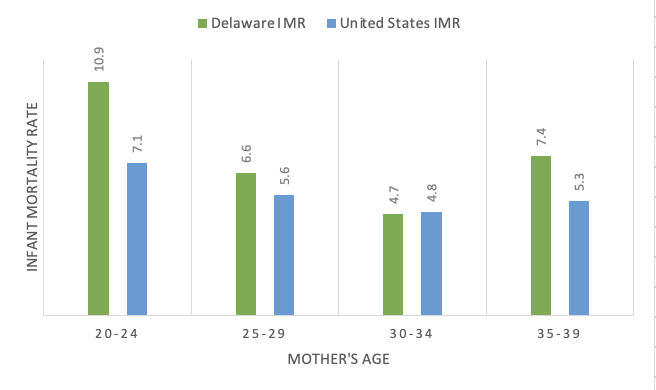
Figure 1: Infant Mortality Rate and Mother’s Ages, Delaware, and the United States, 2020 references the different infant mortality rates by age for women in Delaware compared to the United States. The rate for mothers aged 20-24 in Delaware is at 10.9, which is higher than the national average of 7.1. This age group presented the highest prevalence of infant mortality. Mothers aged 30-34 have the lowest infant mortality rate amongst Delaware mothers at 4.7.
Figure 1
Infant Mortality Rate and Mother’s Ages, Delaware, and the United States, 2020
Note: The graph above displays the IMR for mothers in various age ranges for both Delaware and the United States
Figure 2: Infant Mortality Rate and Mother’s Race in Delaware and the United States in 2020 identifies differences in IMR by Race/Ethnicity of women in Delaware, compared to the United States. Black women in Delaware have a 12.6 IMR, and they have the highest IMR in Delaware, while White women have the lowest IMR, which is 4.8. In 2020, Delaware saw 358 infant deaths in New Castle County, 96 in Sussex County, and 93 in Kent County.
Figure 2
Infant Mortality Rate and Mother’s Race, Delaware, and the United States, 2020
Note: This graph displays the IMR based on Race & Ethnicity of mothers in Delaware and the United States
In Delaware, the City of Wilmington (located in New Castle County) has the highest rates of infant mortality. The IMR in Wilmington is 14.5, compared with New Castle County at 6.6. The non-Hispanic Black community has a higher IMR than average in the City of Wilmington at 16.9, and the value for non-Hispanic White women is not recorded. In this same period, it is shown that the IMR in the non-Hispanic Black community in New Castle County is 12.8, versus 4.6 in non-Hispanic White women, which is a 178% difference.
causes
Preterm Birth
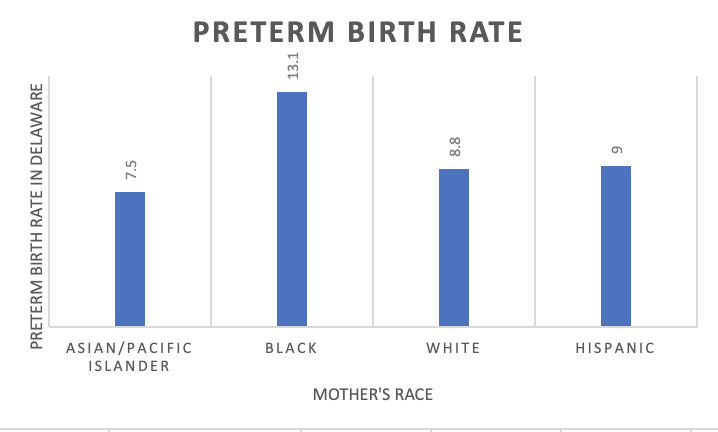
Preterm birth is the leading cause of death for infants. Preterm birth is described as babies born before 37 weeks’ gestation. The preterm birth rate is disproportionately higher for Black women, and in Delaware, the rate is 51% higher than the rate of all other women.
Figure 3
Preterm Birth Rates and Mother’s Race in Delaware, 2020
Note: This graph displays preterm birth rates based on Race/Ethnicity of mothers in Delaware.
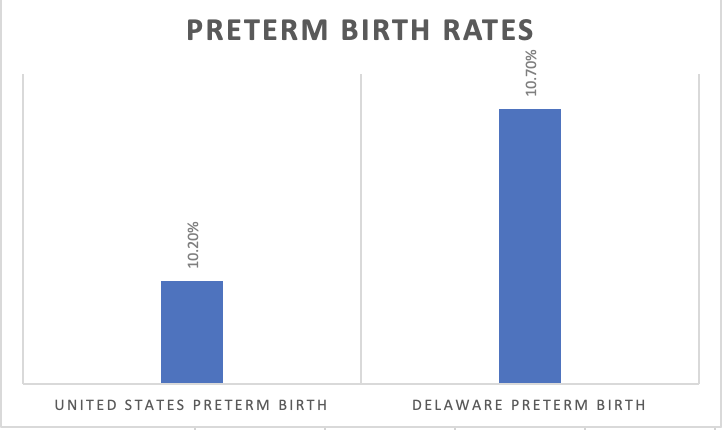
Figure 4
Preterm Birth Rates in Delaware and the United States, 2020
Note: This graph displays the differences in preterm birth rates between the United States and Delaware. Delaware has a higher rate of preterm birth than the United States.
March of Dimes
Low Birth Weight
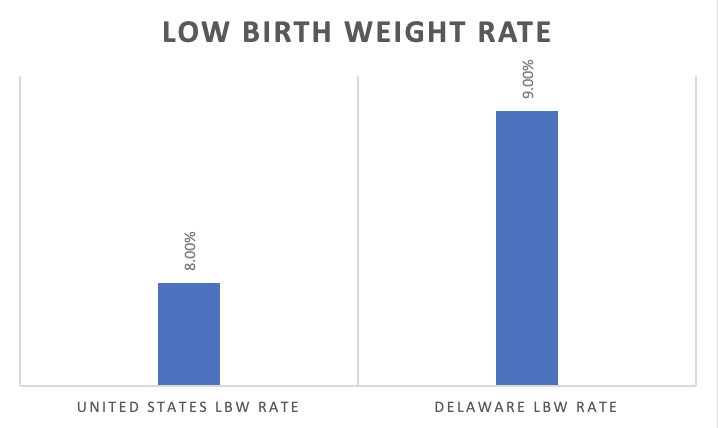
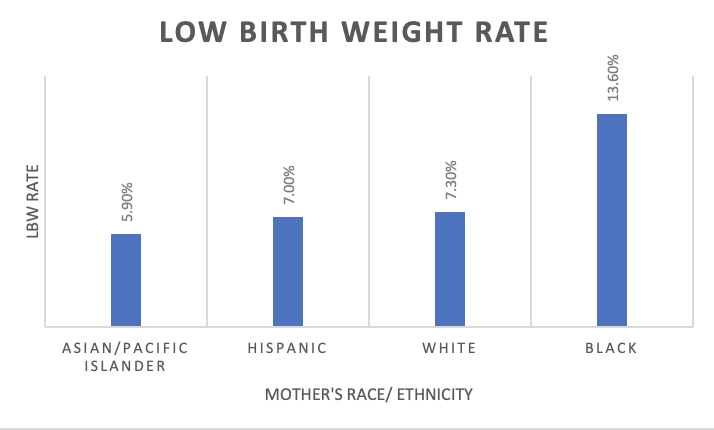
Low birth weight (LBW) is considered to be another large contributor to infant mortality. Babies born at less than 2,500 grams are born at low birth weight. Delaware has a higher rate of babies born at low birth weight than the United States, and the ratings vary between mother’s of different races/ethnicities. Black women in Delaware have the highest rate of LBW deliveries.
Figure 5
Low Birth Weight Rates in Delaware and the United States, 2020
Note: This graph displays the rates of LBW births in the United States and Delaware. Delaware has a higher rate of LBW births than the United States,
Figure 6
Low Birth Weight Rates and Mother’s Race/Ethnicity in Delaware, 2020
Note: This graph displays the rates of LBW based on mother’s race/ ethnicity in Delaware. Black women have the highest rate of LBW deliveries, while Asian/Pacific Islander women have the lowest rate.
Social determinants
The social determinants of health (SDOH) refer to the “conditions in which people live, learn, work, and play”. The pillars of SDOH include education, healthcare access, economic stability, neighborhoods, and community- these factors help shape the prevalence of infant mortality. These determinants are more than sociodemographic risk factors and play a key role in the health of individuals and their communities. They can be explained at an individual, interpersonal, organizational, community, and policy levels.
On an organizational level, availability of and access to medical providers and hospital facilities have proven to have the biggest impact on infant mortality. Assessing a woman’s place of residence during the time of birth is important to understand her access to care. Women in rural or impoverished neighborhoods have a lower “proportion of medical specialists, such as obstetricians and neonatologists, relative to the number of births”. Having less access to these specialists can increase infant mortality. The level of hospital facility is also a risk for infant mortality: Neonatal Intensive Care Units (NICUs) with high-level and high-volume (level III NICU’s) have proven to have lower levels of in-hospital infant deaths).
The community level social determinants of health focus on neighborhoods, concentrated poverty, and racial segregation as risks for infant mortality. There are geographical factors that contribute to infant mortality, and there are some areas that have more protective infrastructures than others, which can help reduce that risk. Those protective factors can also be part of the organizational level of SDOH, such as access to high level treatment centers and an abundance of medical specialists. There is also a correlation between neighborhood/concentrated poverty and higher rates of infant mortality.
The African American community faces the poorest birth outcomes out of all the racial/ethnic groups in the United States. This community sees the highest rate of infant mortality, LBW, and preterm birth, and there is a correlation between racial segregation and infant mortality. They are the “most segregated group in the United States, and they are over-represented in high-poverty neighborhoods”. Since there is an overrepresentation of the African American community in impoverished neighborhoods, there can be worse birth outcomes amongst this group.
At the policy level, there is a perpetual trend of reinforced inequality in education, housing the economy, and criminal justice that creates an environment of discrimination against minorities. Cook conducted an ecological study to find whether structural racism increases individual odds for infant mortality among white and black infants in the US. He used 2010 US Cohort Linked Birth and Infant Death Data Files and looked at the following indicators of structural racism- electoral, employment, and justice system. He compared the proportions of blacks to whites in these indicators and used multilevel logistic regression to assess the relationship between structural racism indicators and infant mortality. His study found that racial disparities in maternal education and incarceration were found to be a risk factor for infant mortality. The study also observed a relationship between income and increased odds for preterm births.
Helping mothers have healthy babies program
Helping Mothers Have Healthy Babies includes definition and structure of the program, identification and management of stakeholders, website creation, education, and a communication plan. The program aims to help educate non-Hispanic Black women of reproductive age in the City of Wilmington[1] on the high risk of infant mortality that is faced by this community. Helping Mothers Have Healthy Babies will produce present a webinar and create a website with access to the live webinar and a recording, along with access to information for doctor’s offices, transportation information, and connection to supplies for mothers and newborn babies.
The first section of the Helping Mothers Have Healthy Babies logic model is dedicated to outlining the program (Appendix A). The first objective is to outline the webinar, website, and survey materials, and create a timeline for their implementation. The timeline will be shared with collaborators. The next objective is to define the program goals and create a mission statement to share with interested collaborators. This objective is important for creating vision for the rest of the program. The collaborators will have a chance to participate in the formation of the mission statement and goals.
The next objective in the program is identification and engagement. Helping Mothers Have Healthy Babies will reach out to interested collaborators, including the March of Dimes, the Delaware Healthy Mother and Infant Consortium, and the Delaware Division of Public Health. Finding interested collaborators is essential for the creation of the webinar. These collaborators will be able to provide insight into what information needs to be presented, and potentially present information on the webinar. Once a group of interested collaborators is established, it will be turned into a formal list of stakeholders, and the collaborators will be updated periodically on the progress of the program.
The next objective is the creation of the website. The website is a key piece of Helping Mothers Have Healthy Babies. The site will include access to the webinar- both when it is streamed live and a recording- as well as access to information about connections to clinics/doctor’s offices for women for pre-and post-natal care, access to transportation information to get to and from these appointments, and a page for women to find resources for supplies needed during and after pregnancy for both mother and baby. The website will have a launch date of July 2021.
After the creation of the site, the formulation of the webinar and surveys can begin. The first objective is to reach out to the interested collaborators about content for the webinar. The webinar is scheduled for August, so the goal is to have 100% of the webinar planned and scheduled with speakers by July. The creation of a survey for the attendees of their knowledge before and after the webinar is an important metric to see if the information provided in the webinar is helpful. The data from the surveys will provide insight for the effectiveness of the webinar and can help shape future initiatives.
The final piece of Helping Mothers Have Healthy Babies is the communication plan. These objectives are essential to the program, since this is how the program will reach the target audience. The main goals of the communication plan are to advertise using emails or brochures in different doctor’s offices, clinics, hospitals, and emergency rooms in the Wilmington area. There will also be a social media initiative for the program as well. Throughout the time of communication initiatives, a list of interested attendees will be formulated from the time they register for the event. This list will be utilized to send updates about the website, webinar, and future events.
[1] City of Wilmington Zip Codes: 19801, 19802, 19803, 19804, 19805, 19806, 19807, 19809
Wilmington, Delaware (DE) Zip Code Map – Locations, Demographics. Wilmington, Delaware (DE) Zip Code Map – Locations, Demographics – list of zip codes. (2016). https://www.city-data.com/zipmaps/Wilmington-Delaware.html.